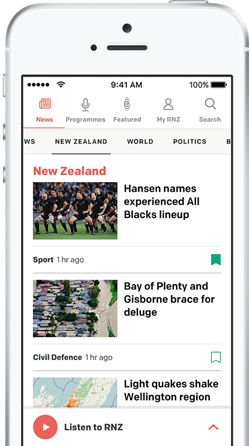
ACT MP Todd Stephenson's Member's Bill has now been redrafted and re-lodged. Photo: RNZ / Samuel Rillstone
ACT MP Todd Stephenson is looking across the aisle for support to change the End of Life Choice Act.
His Member's Bill - lodged in September 2024 - aimed to scrap a requirement for a prognosis of death within six months.
The change was backed by a petition Stephenson accepted the month before - and was supported by party leader David Seymour who championed the original law's passage through Parliament.
The Member's Bill has now been redrafted and re-lodged to include all 25 recommendations from the Ministry of Health's official review of the law three years after it passed, a legal requirement under the original Act (see below for a list of the recommendations).
National's coalition agreement with the ACT Party demands that any changes to the euthanasia law can only be progressed through a member's bill, so Stephenson's bill is their solution.
Given Parliament voted on the original law as a "conscience" issue - with MPs voting according to individual preference rather than along party lines - the same approach is expected this time around.
Stephenson told RNZ he had sent letters to all MPs across Parliament late last week, and while he had not had any responses yet the conversations with MPs so far had been "constructive".
"I think people are more comfortable now that we've had the end of life choice regime in place now for a number of years," he said.
"A number of people across Parliament have had people write to them about their personal stories or have told them about their experiences so, look, I think people are at least willing to listen to the arguments and why some of these changes might be necessary."
"I've had no one specifically say that they're opposed to the changes - but as I said, it's early days."
Member's bills are typically drawn from a biscuit tin at Parliament, so the chances are usually fairly random.
However, a change to Parliament's rules brought in around the time of the last election means that if a Member's Bill gets support from 61 MPs who are not a Minister or Undersecretary, it can skip the usual ballot process. This would require broad support across the Parliament.
Groups opposing the Stephenson's proposed removal of the six-month requirement have raised concerns it could bring New Zealand's approach closer to that of Canada, which had seen euthanasia increase to 2.5 percent of all deaths in Canada in 2020.
Stephenson rubbished the claim.
"Look, I'd say that's completely unfounded. All of the safeguards that are in the current system remain. All we're doing is making a small change to the eligibility to make sure that those who are actually have a terminal illness and do want to choose to die with dignity can do so," he said.
"What we're doing here is really just making some very sensible changes that have been recommended by an independent report, and then also update one very important criteria around eligibility, so that actually more people with a terminal illness can access this and make the decision themselves."
The Ministry of Health review's recommendations include:
- 1. Amend section 10 of the Act so health practitioners cannot raise assisted dying, except as part of discussions about a person's treatment and end-of-life care options.
- 2. Add a provision to the Act stating that nothing in section 10 prevents the publication or provision of public information about assisted dying, or the assisted dying service.
- 3. Clarify the threshold for when the process must stop if the practitioner detects pressure.
- 4. Clarify in the Act that the person must be competent and informed to make a decision at key points in the process where the person is making a decision about assisted dying. This includes at the point of assessments, and on the day of the assisted death. Also, specify some factors that by themselves are insufficient to find that a person is not competent to make an informed decision.
- 5. More clearly set out in the Act the core duties that practitioners must fulfil to ensure that the person accessing assisted dying is eligible, actively seeking and consenting to it, is competent to consent to it, and that this consent is provided free from pressure from others. More clearly define ongoing procedural requirements on practitioners that may constitute steps towards the practitioner's core duties.
- 6. Clarify the enforcement pathways for breaches of particular requirements in the Act, linked to the core duties and requirements as referenced in recommendation 5. (The report sets out three pathways)
- 7. Amend section 36 of the Act to be more specific about what details about an assisted death cannot be published. (
- 8. Add a provision stating that a person who is found ineligible for assisted dying, or who has rescinded their request to exercise the option of assisted dying, must submit a new request if they wish to reapply at a later date.
- 9. Add a provision that enables the functions, responsibilities, and duties of an attending practitioner to be transferred to another attending practitioner, provided that the new attending practitioner agrees to take on the role. When the new attending practitioner takes on the role, they must advise the Registrar. The provision would state that the role of attending practitioner cannot be transferred to the independent medical practitioner.
- 10. Add a provision that establishes a six-month period within which a person is able to set a date and receive an assisted death, following approval by the Registrar. This six-month period would commence from the date when the Registrar determines that compliance requirements have been met. Further, add a provision providing that an additional six-month extension of this period may be granted by the Registrar if at the end of the initial six-month period.
- 11. Remove the requirement for the person to choose a date and time for administration of the medication after they have been found eligible. Remove references in the Act to the "date initially chosen". Remove the requirement to choose a method for administration of the medication after a person has been found eligible. Remove the 48-hour rule and related provisions requiring the Registrar to check compliance and confirm compliance with requirements in the Act.
- 12. Expand the regulation-making power in the Act to state that regulations must be made to specify: what a practitioner is required to do when they 'examine' a person as part of the assessment process; the methods for administration of the medication; requirements for the management of prescriptions made under the Act. Remove the following provisions from the Act (on the basis that these will be covered by regulations instead): The list of methods for administration of the medication; Provisions involving the way that prescriptions are managed.
- 13. Amend the Act to separate conscientious objection provisions from how a person accesses the Assisted Dying Service, and clarify obligations on all health practitioners to provide details of the Assisted Dying Service if a person makes a request
- 14. Amend the Act to set out what practitioners are able to conscientiously object to, that conscientious objection does not override a practitioner's duty to act in accordance with the Code of Health and Disability Services Consumers' Rights, and specific actions that health practitioners must take to facilitate continuity of care.
- 15. Require care facilities to provide reasonable access to assisted dying to those who request it, particularly for those where the facility is the person's home ('care facilities' means public hospitals, private hospitals, hospices, residential aged care facilities, disability residential care facilities, and rest homes or other similar facilities where care is provided to a person.
- 16. Amend the Act to more clearly articulate that a practitioner should not be treated any more or less favourably than any other similarly qualified health provider by an employer, regardless of whether they provide assisted dying services or not.
- 17. Require medical and nurse practitioners providing assisted dying services to have held a practising certificate for a minimum period of five years.
- 18. Add an explicit requirement that practitioners who provide assisted dying services must complete required training, including any refresher training, which must cover their duties under the Act.
- 19. Allow the third assessment (to determine competence) to be provided by a psychiatrist (as currently set out in the Act), or a health practitioner with specialist vocational registration in an area set out by the Director-General of Health.
- 20. Allow nurse practitioners to fulfil all of the responsibilities that are currently undertaken by an attending practitioner, but not fulfil the role of the independent medical practitioner.
- 21. Amend section 25 of the Act to make the SCENZ Group an expert advisory group which provides specialist advice and support for practitioners, the Ministry of Health, and Health New Zealand on the processes under the Act. The name of the SCENZ Group would be changed to reflect its functions - for example, the Assisted Dying Expert Advisory Group.
- 22. Amend section 27 of the Act to require the Registrar to make a determination of compliance based on whether the documentation and information provided by practitioners demonstrates compliance with the requirements under the Act.
- 23. Amend section 26 of the Act to clarify that the purpose of the Review Committee is to: consider all documentation produced during the course of individuals seeking and/or receiving an assisted death; determine whether the information recorded shows satisfactory compliance with the requirements of the Act; as necessary, make recommendations to the relevant organisations and entities to support quality or practice improvements, and indicate where information may be insufficient to demonstrate compliance with the requirements of the Act.
- 24. Set out in the Act specific immunities for the Registrar and the Review Committee. The Act would also specify that judicial review is available as an accountability pathway.
- 25. Add a provision setting out the role of Health New Zealand in the Act. This would see Health New Zealand undertake a number of functions to support the operation of assisted dying as a health service.
The review also makes a range of other minor changes to improve clarity, and contains more detail about the way the above recommendations would work.
Sign up for Ngā Pitopito Kōrero, a daily newsletter curated by our editors and delivered straight to your inbox every weekday.